Good Night Sleep is One Way to Boost the Immune System and Protect Yourself
By: UthayanThurairajah
Coronaviruses (CoVs) are RNA viruses infecting both humans and animals; this infection involves the respiratory, gastrointestinal, and central nervous system (Cui, J. et al., 2019). The Middle East respiratory syndrome (MERS) coronavirus and Severe acute respiratory syndrome (SARS) coronavirus are dangerous and deadly and have made many deaths in the past twenty years. The current outbreak was discovered in Wuhan, China; this highly contagious disease has spread throughout China and other countries (Huang, C., et al., 2020).There is a lack of a specific treatment for COVID-19, even though Corticosteroid therapy, antiviral therapy, and mechanical respiratory support have been applied.
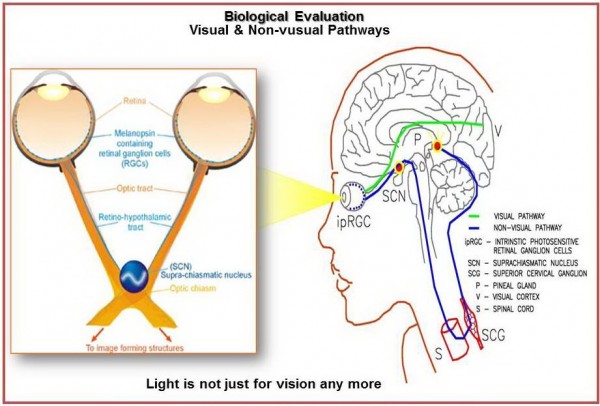
Melatonin (N-acetyl-5-methoxytryptamine) is a bioactive molecule with an array of health-promoting properties; melatonin has been successfully used to treat sleep disorders, delirium, atherosclerosis, respiratory disease, and viral infections (Reiter, R. et at., 2020). Previous researches have been documented the positive effects of melatonin in alleviating acute respiratory stress induced by the virus, bacteria, radiation, etc. (Wu, X., et al., 2019). We can examine the data showing that melatonin will have supportive adjuvant benefit in administering COVID-19 caused pneumonia, acute lung injury (ALI), and acute respiratory distress syndrome (ARDS).
The rationale for Melatonin Use
Melatonin does not destroy viruses, but it has indirect anti-viral actions (Reiter, R. et at., 2020) due to its anti-inflammation, anti-oxidation, and immune-enhancing features (Anderson, G. et al., 2015). There are conditions in which melatonin suppresses the features of viral infections. In mice whose central nervous system is infected by a virus, the use of melatonin caused less viremia, reduced paralysis, and death, and decreased virus load. In previous respiratory syncytial virus models, melatonin caused down-regulation of acute lung oxidative injury, pro-inflammatory cytokine release, and inflammatory cell recruitment. These findings, along with those recently summarized by Reiter et al. (2020), support a rationale for melatonin use in viral diseases. Also, melatonin’s anti-inflammation, anti-oxidation, immune-enhancing actions support its potential attenuation of COVID-19 infection.
Melatonin & anti-inflammation
Melatonin exerts anti-inflammatory effects through various pathways (Hardeland, R. et al., 2018). The anti-inflammatory effect of melatonin involves the suppression of NF-κB activation in Acute respiratory distress syndrome (ARDS) (Sun, C.-K., et al., 2015). Melatonin reportedly down-regulate NF-κB activation in T cells and lung tissue (Pedrosa, A.M. et al., 2010). The data supports the potential anti-inflammatory action of melatonin. Inflammation is commonly associated with elevated production of cytokines and chemokines, while melatonin causes a reduction in the pro-inflammatory cytokines. There may be, however, some concerns about the potential pro-inflammatory actions of melatonin when used in very high doses or under suppressed immune conditions where it may induce an increased production of pro-inflammatory cytokines, IL-1β, IL-2, IL-6, IL-12, TNF-α, and IFN-γ (Carrascal, L., 2018). Conversely, in Acute Lung Injury (ALI) infection models, melatonin presents with anti-inflammatory and protective action (Huang, S.H. et al., 2010).
Melatonin & anti-oxidation
The anti-oxidative impact of melatonin cooperates with its anti-inflammatory actions by regulating anti-oxidative enzymes (e.g., superoxide dismutase), down-regulating pro-oxidative enzymes (e.g., nitric oxide synthase) (Reiter R.J. et al., 2020). In ALI/ARDS patients, especially when the disease is advanced and in patients treated in intensive care units (ICUs), severe inflammation, hypoxemia, and mechanical ventilation with high oxygen concentrations inevitably increase oxidant generation locally and systematically (Tamura D.Y., 2002). Accordingly, we speculate that excessive oxidation also is likely involved in COVID-19. The extensive studies of Gitto et al. (2005), who used melatonin to treat newborn infants with respiratory distress, has documented the anti-oxidant and anti-inflammatory actions of melatonin in the lung. Thus, it is likely that the application of melatonin would be beneficial in controlling the inflammation and oxidation in coronavirus infected subjects.
Melatonin & immunomodulation
When the virus is inhaled and infects respiratory epithelial cells, dendritic cells phagocytose the virus and present antigens to T cells. Both the pathogen (CoV) and cell apoptosis trigger and amplify the immune response. The exacerbation of cytokine production, excessive recruitment of immune cells, and the uncontrollable epithelial damage generate a vicious circle for infection-related ALI/ARDS (Yang C.-Y. et al., 2018). Melatonin uses regulatory actions on the immune system. It improves the immune response by growing reproduction and maturation of natural killing cells, T and B lymphocytes, monocytes, and granulocytes, in both bone marrow and other tissues (Miller S.C., at al., 2006).
The pathogen, including a virus (CoVs), triggers NLRP3 activation to amplify the inflammation. It supports the use of melatonin in ALI/ARDS when inflammation is most severe. Inflammasome NLRP3 is correlated to lung diseases caused by infection, including influenza A virus, syncytial virus, and bacteria (Tate, M.D., et al., 2016). The ability of melatonin in regulating NLRP3 has been proven in radiation-induced lung injury, allergic airway inflammation, and oxygen-induced ALI and LPS-induced ALI models, in which melatonin reduced the infiltration of macrophages and neutrophils into the lung in ALI due to the inhibition of NLRP3 inflammasome (Zhang, Y., et al., 2016).
Melatonin effects in cytokine levels
The use of melatonin showed promising results regarding the attenuation of circulating cytokines levels. In a randomized controlled trial, an 8-week oral intake of 6 mg/d melatonin caused a notable decrease in serum levels of IL-6, TNF-α, and hs-C-reactive protein (hs-CRP) in patients with diabetes mellitus and periodontitis (Bazyar, H., et al., 2019). A new meta-analysis of a total of twenty-two (22) randomized controlled tests suggested that additional use of melatonin is produced a significant reduction of TNF-α and IL-6 level (Zarezadeh, M. et al., 2019). The clinical evidence hints that the use of melatonin as a supplement effectively reduce the levels of circulating cytokines and may potentially also lower pro-inflammatory cytokine levels in COVID-19 patients.
Melatonin & safety
When considering the use of melatonin to treat COVID-19, the safety of the melatonin is of utmost significance. As reviewed previously, short-term use of melatonin is safe, even in those given high doses, and the reported adverse effects are limited to occasional dizziness, headache, nausea, and sleepiness; in general, melatonin’s safety in humans is very high (Andersen L.P.H. et al., 2016). In clinical trials, doses of 3 mg, 6 mg, and 10 mg of melatonin oral intake by patients in ICU showed satisfactory safe (Bourne, R.S., et al., 2008). The safety of melatonin has been verified in many human studies. The effect of melatonin, when given to COVID-19 patients, should be carefully monitored.
Conclusion
The possible useful outcomes of melatonin to enhance the immune system to fight in COVID-19 in anti-inflammation, anti-oxidation, immune response regulation has been proved in respiratory disorder models induced by infections and associated complications. Melatonin has a high safety profile. Although the direct evidence of melatonin application in COVID-19 is unclear, both its use in experimental animal models and studies on humans has continuously documented its efficacy and safety, and its use by COVID-19 patients predictably would be highly beneficial.Therefore, good night sleep is one way to boost the immune system and protect yourself during this Covid-19 Pandemic.
Uthayan Thurairajah, Ph.D., RSE, LC, P.Eng.,FEC, is a Project Manager at WSP with over twenty years of experience in Electrical Engineering and Lighting field, and he also holds a Lecturer position at Ryerson University & professor at Centennial. Uthayan is a member of several Canadian and international professional association including Professional Engineers Ontario (PEO) and Association for Prevention Teaching and Research (APTR). He has worked on multi-disciplinary lighting and electrical projects for various clients. He researches the subject of light and lighting and taken part in several projects. He also has extensive research experience in the value of lighting design in the mental, emotional, and social well-being of a person. He is a frequent presenter and author of lighting design & health. He is passionate about integrating science and health into the lighting design.